Look at Figure 1

Figure 1:
Image source:
http://www.sollis.co.uk/wp-content/uploads/2016/10/equity-vs-equality.jpg
In Figure 1, all three children are of equal height.
But,
they cannot reach the fruits,
Because of,
the terrain’s unequalness.
They need help. But, the help each one requires is different. They need boxes of different heights.
By helping them with boxes of “appropriate height”,
all three can reach the fruits.
This is equity:
Providing help appropriate to the degree of help needed.
As we can see the degree of help needed varies not due to inherent biological differences.
It is due to reasons outside their control.
When we find group differences due to reasons other than biological causes such as age, sex, or genetic makeup, we are talking about equity.
Therefore,
- Health equity is political.
- Health equity is about social justice.
- Health equity is about moral values.
Hence,
- Health inequities are unfair,
- Health inequities are unjust,
- Health inequities are avoidable.
The above words are from Margaret Whitehead’s definition of health inequity.
- Health inequities are not natural,
- They are
- socially produced,
- and sustained by deeply entrenched unjust social systems.
Therefore,
talking about health inequity goes beyond science.
Science alone cannot determine which inequalities become inequities.
Kawachi et al. use the term, “normative judgement”.
It requires,
- One’s theories of justice,
- One’s theories of society,
- One’s reasoning for how the inequity arose in that particular situation.
Now, we will look at a real-world scenario.
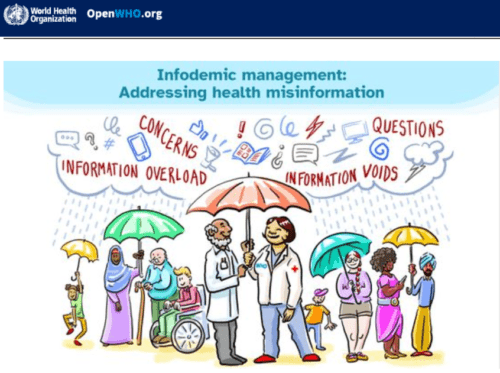
Look at Figure 2.
It depicts deaths due to the COVID-19 virus reported in England.
We can see that deaths were higher in the poorest areas.
It is a classic case of health inequity.
This social gradient surfaced all over the world.
Figure 2:
(Source: BBC News, 2020)
Vaccine equity
The covid-19 pandemic brought the word “equity” right in front of us. We saw one classic example above.
Vaccine equity is another classic example.
Rich countries took most of the vaccine; they gave the poorer countries what was left: Leftovers.
Here is how Dr Mike Ryan explained this unfair global vaccine distribution for Covid19.
What is health equity?
WHO definition:
Health equity refers to “the absence of unfair and avoidable or remediable differences in health among social groups”. (WHO, 2010, Page 12).
This absence of unfair and avoidable differences is with regard to the outcome.
Irrespective of whatever the differences that we find among different social groups, all should be able to achieve an equal outcome.
The key phrase here is the “health outcome”.
We need to ensure all will reach an equal outcome.
Now, let us look at the following definition.
Robert Wood Johnson Foundation (RWJF) Definition:
“Health equity means everyone has a fair and just opportunity to be as healthy as possible”.
The RWJF has added another sentence to the above definition;
That is to translate the concept into an actionable one; it goes as follows;
“For measurable purposes, health equity means,
- Reducing and ultimately eliminating disparities in health and,
- Its determinants that adversely affect the marginalised and excluded groups”.
What is health inequity?
Health inequity is a difference in a health situation that is socially produced, systematic in its distribution across the population, and unfair (WHO, 2010, page 12).
Health inequities are avoidable.
This definition guides us to more focused actions.
The relation between health inequity and health inequality (disparity)
Health inequity is a sub-type of health inequality.
Health inequality (disparity) refers to the difference in a health outcome and its determinants between population groups as defined by social, demographic, environmental, and geographic variables. (Source: CDC: Mortality and Morbidity Weekly Report, 2011).
All health inequities are health inequalities;
But,
all health inequalities are not health inquities.
Why all health inequalities are not health inequities?
Let us explore this confusion with an example;
Look at Figure 3 below.
It depicts the incidence of Downs Syndrome by women’s age.
We can see that the risk of having a baby with Downs syndrome increases with women’s age.
This is a health disparity.
But,
it is a biological variation. So, it is not a health inequity.

Figure 3
In short, health equity is a valued judgement.
Health equity is a value judgement on health equality.
W-C Chang
Some authors recognise health inequity as “needs-adjusted health inequality”.
The following two illustrations compare equity and equality.
If we consider equality only, we give three boxes of equal height to the three children. Obviously, it does not ensure equal opportunities for all three children (Figure 4).
The following two illustrations summarise the difference between health equality and equity.
Illustration 1:
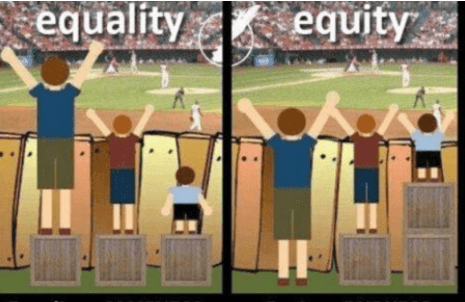
Figure 4:
Illustration 2:

Figure 5
How to determine a health inequitable situation
Deciding a particular health disparity as a health inequitable situation is not an objective description. It needs a moral judgement as we already saw earlier.
Step 1:
W.C. Chang proposes asking the following question for a value judgement.
- Can you attribute the observed variation in health status to a biological factor?
If you do not have any plausible biological explanation, then, it could be due to one or more non-biological factors such as social, cultural, economic, and political.
If that is the case, such differences are,
- Unnecessary,
- avoidable.
Step 2:
If the observed difference is unnecessary and avoidable, then we ask the second question.
- Is this inequality unjust and unfair?
Now, the discussion can become debatable.
Consider the following scenario.
If we compare the life expectancies at birth in Russia and China with that of Western societies, it is clearly a difference in political ideologies.
On the other hand, if we attribute the difference to either economic exploitation or colonialism by powerful countries, then we could say that there is health inequity. In addition to this reason, it could also be other reasons such as corruption.
Types of equity:
W-C- Chang mentions two terms to recognise inequitable situations;
- Horizontal equity: Is there a “breach to equal treatment to equal people?”
- Vertical equity: Is there an unequal treatment to unequal needs by the same authority?”
Horizontal equity
Horizontal equity refers to “equal access or treatment to equal needs regardless of socio-economic factors”.
In other words, “all equals must be treated equally”.
Horizontal equity = “Equal treatment for equal need”.
All people with the same health conditions must be treated equally irrespective of their socioeconomic or socially constructed differences. In most countries, primary healthcare services show this horizontal equity.
Research reveals that horizontal inequity exists in OECD countries and it is pro-poor; on the other hand, specialized services and dental care are pro-rich.
Examples of health equity:
- Equal quality of healthcare for the same health needs irrespective of differences of socio-economic differences
- Equal access for equal health needs; e.g. same waiting periods for the same health needs.
- Equal healthcare services for areas with equal (age and gender-adjusted) standardised mortality rates
What affects horizontal equity?
Income, educational level, age, gender, place of residence, place of birth, and ethnicity influence horizontal equity.
Assuring horizontal equity alone is not enough. why?
We need to ensure vertical equity as well.
Vertical equity
Vertical equity refers to “appropriate unequal access to health care for people with different needs”. In other words, people with greater clinical needs should have more access to care than those with lesser clinical needs.
“Vertical equity: “Unequal treatment for unequal need”.
In other words, “all un-equals must be treated differently”; people with more needs must receive more support. Keep in mind that those in greater need do not seek attention.
How do health inequities arise?
Health inequities arise due to unequal exposure and vulnerability to illnesses as a result of our position on the social ladder. We, as a society, assign, usually, social positions according to income level, education attainment, gender, ethnicity etc.
The 2010 WHO conceptual framework published by Solar and Irvin (Figure 6) describes the mechanisms of how social stratification happens and it results in unequal health outcomes.
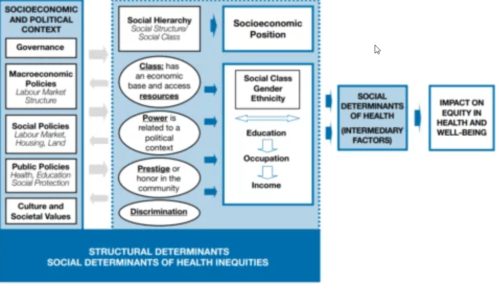
Figure 6
Since all these mechanisms are socially produced, health inequity is unfair, unjust, and avoidable.
Structural determinants
(Social determinants of health inequities):
Figure 6 illustrates the 2020 WHO framework. It includes much larger “structural determinants” and smaller “intermediary factors”.
The former is called “social determinants of health inequities” and the latter is called “social determinants of health”.
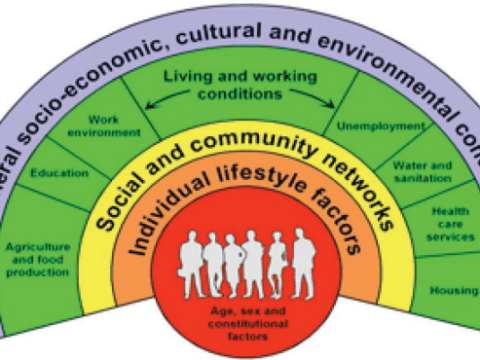
Rainbow model
Figure 7 depicts another useful mode that illustrates the same health inequity-causing mechanisms: The “Rainbow model”.
Dahlgren and Whitehead published this model in 2006.
This model divides the health inequity-causing mechanisms into four layers according to the degree of influence. For example, the biggest influence comes from the outermost layer and it can negate any achievement of the inner layers.
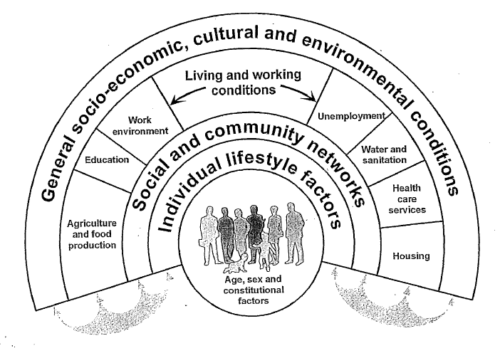
Figure 7: Dahlgren and Whitehead’s “rainbow model”
(Source: Dahlgren & Whitehead, 1991.
Policies and Strategies to Promote Social Equity in Health. Stockholm, Sweden: Institute for Futures Studies)
This post favours the 2010 WHO framework; hence let us explore it more.
We will begin the journey from the left-most column of the framework: “Socioeconomic and political context” (Figure 6).
The dominant political system as a structural determinant:
There is ample evidence that capitalism and its neo-liberal policies and strategies, the dominant political ideology in the world, “nurtures” inequality.
For example, the richest 10 per cent in the USA own 74 per cent of wealth. In the UK, it is 44 per cent.
More evidence is necessary to understand better how political and market forces fuel health inequity.
The political structure is the core determinant of society’s well-being.
It shares every other determinant of health inequities and well-being.
In this TED Talk, Nick Hanauer, an entrepreneur and venture capitalist, succinctly argues the limitations of the neoliberal economic mechanism.
It does not mean that the other ideologies such as Marxism that restrict human dignity ensure health equity and wellness.
The capitalism-marxism debate began as far back as the 19th century with the onset of the Industrial Revolution.
As a guide, in 1891, Pope Leo XIII released the then-revolutionary masterpiece, Rerum Novarum.
We cannot promote health equity ignoring the political ideology dominant in society in consideration.
In 2006, the European strategies for tackling social inequities in health emphasised the importance of improving “political and market democracy” to empower the least powerful.
And, the 2010 WHO framework also stresses that “the political nature of the endeavour needs to be an explicit part of any strategy to tackle social determinants of health” (page 7).
Evidence exists that a high level of democracy reduces the impact of unfavourable economic and trade policies on infant mortality.
Whatever political choices we make, we can use the 1948 Universal Declaration of Human Rights as a guide to promoting health equity.
Policy context:
The political choices we make become a reality through passing legislation by the people’s representatives at the political bodies. Then we formulate policies. Our values guide policy choices and values can either be implicit or explicit.
The WHO framework outlines three types of policies: Macroeconomic, social, and public.
Macroeconomic policies cover the following areas:
Fiscal, monetary, trade, the balance of payments, and the labour market.
The social and public policies include land, housing, health, education, social welfare, water and sanitation etc. It also includes pandemics such as COVID-19.
The framework emphasises the importance of tackling structural determinants as well while crafting policies. That is the single most significant lesson according to the framework.
We must not design policies only to address much smaller intermediary factors of health inequity (page 7).
This requires intersectoral action and social participation and empowerment at every level: Global, national, and local.
Governance:
Governance is the way a society organises itself to make decisions and implement those. It operates at every level: household, local, community, municipality, provincial, national, and global. It also includes all sectors: The state, civil society, and the private sector.
We can measure the effectiveness of governance mechanisms by creating indicators along the following themes;
- Perceived and objective social needs,
- Civic participation,
- Accountability,
- Transparency in public administration,
- Other laws, rules, and practices that set limits.
Cultural and social values and norms:
The dominant societal values and norms in any society shape the nature of the policies the society chooses. These values and norms may either be implicit or explicit. For example, our values towards the elderly, gender, sexuality and sexual orientation, race and ethnicity, and those living with physical and mental disabilities guide the policy options we adopt.
The above forces create a social hierarchy.
The above forces create a social hierarchy by stratifying community members into groups. We call this process social stratification.
It occurs through the systematic unequal distribution of wealth, resources, power, prestige, and discriminatory practices (The WHO Framework, 2010. Page 20).
Power needs special attention. How does power become unequal?
This video clip illustrates how power originates and what we can do about it.
Due to this unequal distribution, the higher-ups in the social ladder enjoy a disproportionately higher share than those on the lower down in the social ladder.
Discriminatory practices also contribute to the stratification process.
For example, assigning a lower position to women brings them down in the social location.
This depends on society’s value system.
As a result, this stratification occurs in relation to income level, education, level, gender, ethnicity etc.
Social position decides our vulnerability.
These different social locations lead to health inequities through differential (unequal) exposures and vulnerability (or susceptibility) to diseases and health conditions and unequal consequences of diseases and health conditions across different social groups.
Let us see how it happens.
Diderichsen, Finn, Timothy Evans, and Margaret Whitehead (2001) dissect these mechanisms under three headings.
Unequal exposure to diseases
Lower social positions are associated with unhealthy housing and workplace conditions that may lead to greater exposure to toxic substances and disease conditions.
This unequal exposure to higher risk can deepen throughout their lives with time from “womb to tomb” (life course influence). This is because either advantages or disadvantages accumulate over time even from generation to generation.
Unequal vulnerability to diseases
Those in lower social positions may face more than one risk factor. As a result, the impact of one risk factor can be much more severe on them in the presence of other risk factors than those in upper social positions.
Think of the COVID-19 virus. Its impact on lower social positions was more severe; more who were in lower social positions died of the virus when compared to those in upper social positions.
Unequal socioeconomic consequences of ill health
When those in lower social positions face a chronic disease or any Catastrophic health situation, its impact on their lives will be much more severe than its impact on those in higher social positions.
Intermediary factors
(Social determinants of health)
The structural determinants, discussed above, directly influenced intermediary factors(social determinants of health) (Figure 8).
Those factors operate in our daily living and work conditions and places where we are born, grow, and age.
The quality of such conditions is determined by our assigned social positions; the lower the social position on the social ladder, more the unfavourable conditions become.
In the “rainbow model”, these determinants fall into Layer two.
The framework identifies the following elements as intermediary factors;
- Local physical environment (material circumstances): living and working conditions, neighbourhood environment, healthy food availability, affordability, accessibility etc.
- Local psychosocial environment: stressful living, job stress, work-life balance etc.
- Behavioural and biological factors: Physical activity opportunities, smoking and alcohol and other substance abuse.
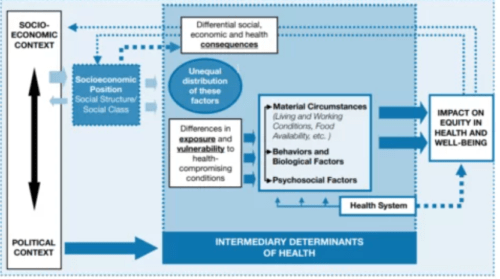
Figure 8: Intermediary factors
Our physical environment matters critically; evidence suggests that “one’s zip code is more important than the genetic code”.
The physical environment includes housing, air quality, neighbourhood, green space, built environments, transport systems, workplaces, schools, healthcare settings, social, private, and public places, government institutions etc.
These also include income and wealth, physical environment, public safety, social environment, transportation, education, employment, health systems and services, and housing.
Health system as an intermediary factor
This framework departs from previous models by recognising the health system as a separate element of social determinants of health because it can modify the intermediary factors to some extent.
Life course perspective as a determinant
The impact of health inequities varies with the age we are in. For example, the health inequities’ impact on early childhood can carry with us as we age.
This is because early “insults” to our body systems may not change through later experiences. This phenomenon is known as “biological programming”.
The association between low birth weight and the later appearance of coronary heart disease is explained through this approach.
Another theory related to the life course perspective is that either the risk factors or promotive factors “accumulate” as we age.
However,
we have developmental milestones, such as teenage, when the health inequity impact becomes more pronounced than in other periods.
According to this “accumulation of risk” model, the damage to our body systems increases cumulatively with time (2010 WHO Framework, page 18).
Social cohesion and social capital
The framework places social cohesion and social capital in an unusual place, in-between structural determinants and intermediary factors. The development of social capital depends on the extent of citizen participation.
How to advance health equity?
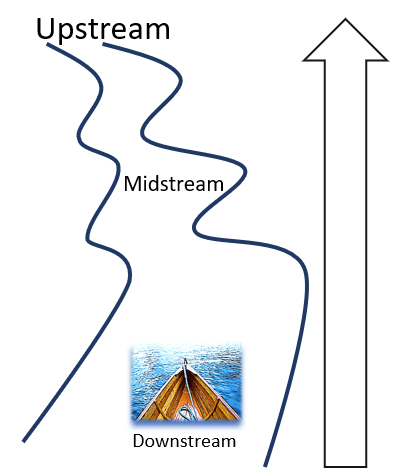
To advance health equity, we have to upstream. However, we can find many entry points while sailing along downstream and midstream as well.
I prefer using the following roadmap.
I prefer using the following Public Health Agency of Canada’s 2018 road map. It captures the essence of health equity concepts and principles.
- Adopt the human rights approach to act upon structural determinants and intermediary factors.
- Intervene across the life course with evidence-based policies.
- Intervene in both downstream and upstream situations.
- Deploy both targeted and universal approaches.
- Address both material issues and sociocultural elements of power, prestige, and exclusion.
- Implement a “health in all” approach.
- Carry out monitoring and evaluation.
In addition to the above, the following strategies must be necessary to elevate health equity in the public health agenda.
Measure it
If we do not measure, we do not know. Assumptions become harmful. That should the be first step. We need to disaggregate data by the health inequity determinants discussed above.
We have excellent precedents.

WHO launched this tool in April 2023. It aims to make disaggregated data more accessible to everyone.

This is managed by the Martin School of the University of Oxford. All data viz and text are freely available for any purpose.

SDG tracker monitors Sustainable Developmental Goal 17 indicators.

This tool gives us up-to-date Health inequalities in data. It is user-friendly and customisable.
Need a paradigm shift:
- From a wealth economy to a well-being economy
We know that our societal values and norms shape our political structure and the policies we adopt. Therefore, we need a paradigm shift in our values. We must value a well-being economy, not a wealth economy.
The WHO has already set up a Council on the Economics of Health for All. It aims to transform the existing paradigm, “good health for a good economy” to “a good economy for good health”.
“A good economy for good health;
Not “a good health for a good economy”
The Council sets out three fundamentals;
- Health and the economy are interdependent,
- Health for all is critical for overall resilience and stability in economies worldwide,
- Shaping public and private investments in health is essential.
The well-being economy movement:
The well-being economy movement network, which began in 2018 in Scotland, Finland, and New Zealand, is gaining traction. In this TED Talk, Nicola Sturgeon, who served as First Minister of Scotland and Leader of the Scottish National Party (SNP) from 2014 to 2023 argues the limitations of the GDP as an indicator and the need to choose alternate indicators to measure the wellbeing economy.
Why?
What we measure as a country’s success matters; it drives political focus. it drives public activity. We will go after wealth, not on well-being if we use the GDP as the indicator.
GDP cannot measure well-being. It measures the output of all work. It cannot measure whether the work is fulfilling and worthwhile. For example, it puts value on illegal drug consumption but not on unpaid care.
GDP measures the output of work that is even damaging to us, and the planet.
https://www.facebook.com/groups/upstreamingpublichealthforum/permalink/962278241683625/
- See the forest for the trees
When we focus on individual well-being only, we fail to see the population’s well-being. It is akin to seeing only one tree because then, we cannot see what the forest looks like. It is different. Geoffrey Rose demonstrated it using data from public health. He showed that the causes of disease incidence in a population are different from the causes of cases. Without that shift in our thinking, we cannot upstream to advance health equity.
Address determinants at all levels
Addressing only one level of determinants does not close the inequality gap permanently. It requires interventions at all levels of determinants.
We can consider the 2011 Rio Political Declaration of Social Determinants of Health as the highest global level commitment. We need to explore this further.
Create a best Practices repository
We can also find excellent documents and web portals that curate best practices aimed at advancing health equity. Following are a few of those;
- 2013 Health Scotland document provides an excellent list of interventions to address structural determinants of health inequities at all three levels.
If you have read this far and if you are aware of such repositories, I am inviting you to send them so that I can make this post more informative.
Communicate creatively
Communicating health equity concepts is hard. We need to use creative methods such as storytelling, cartoons, and creative art etc. Fortunately, we have excellent tools and guides for use. Some of those are as follows;
- Storytelling and illustrations
This parable is being used in many situations and articles to describe what upstreaming public health refers to. The story goes as follows;
” I am standing by the shore of a swiftly flowing river,
and I hear the cry of a drowning man.
So,
I jump into the river,
put my arms around him,
pull him to shore,
and apply artificial respiration.
When he begins to breathe,
there is another cry for help.
So,
I jump into the river,
reach him,
pull him to shore,
apply artificial respiration,
and then just as he begins to breathe,
another cry for help.
So,
back into the river again;
another cry!
Again and again,
without end,
goes the sequence.
You know I am so busy jumping them to shore,
doing the same,
that I have no time to see who the hell is upstream pushing them all in”.
Together with the above parable, several public health agencies have created excellent illustrations;
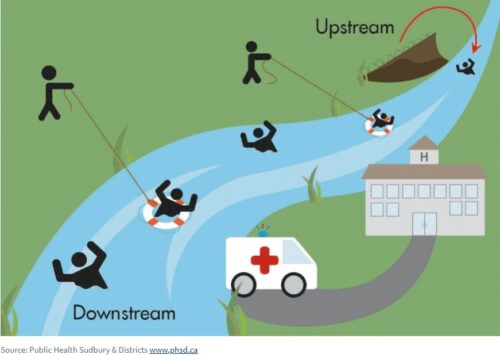
Irving Zola’s “Upstream-downstream parable”; Source: Sudbury and Districts public health

Moving upstream; Source: NCCDH website
- Illustrations and cartoons
- A fence or an ambulance illustration and Joseph Malins’ poem
The cartoon below appeared in the Iowa Health Bulletin in 2012 together with Joseph Malins’ poem about “A Fence or an Ambulance”.

This Joseph Malins’ poem appeared in the Iowa Health Bulletin published in 1912.
The poem is as follows;
The poem relates to an imaginary city. The city council and citizens debate about what to do with the falling people from the cliff.
‘Twas a dangerous cliff, as they freely confessed,
Though to walk near its crest was so pleasant:
But over its terrible edge there had slipped
A duke and many a peasant;
So the people said something would have to be done.
But their projects did not at all tally:
Some said, “Put a fence around the edge of the cliff”
Some, “An ambulance down in the valley.”
But the cry for the ambulance carried the day.
For it spread to the neighbouring city:
A fence may be useful or not, it is true,
But each heart became brimful of pity
For those who had slipped o’er that dangerous cliff,
And the dwellers in highway and alley
Gave pounds or gave pence, not to put up a fence,
But an ambulance down in the valley.
“For the cliff is alright if you’re careful,” they said,
“and if folks even slip or are dropping,
it isn’t the slipping that hurts them so much
as the shock down below-when they’re stopping,”
So day after day when these mishaps occurred,
Quick forth would the rescuers sally
To pick up the victims who fell off the cliff,
With their ambulance down in the valley.
Then an old man remarked,
“it’s a marvel to me
that people give far more attention
to repairing results than to stopping the cause,
when they’d much better aim at prevention.
Let us stop at its source all this mischief, cried he.
“Come, neighbours and friends, let us rally :
If the cliff we will fence, we might almost dispense
with the ambulance down in the valley.”
“Oh, he’s a fanatic…” the politicians rejoined:
“dispense with the ambulance Never!
He’d dispense with all charities, too, if he could:
no, no! We’ll support them forever.
Aren’t we picking up folks just as fast as they fall?
And shall this man dictate to us? Shall he?
Why would people of sense stop to put up a fence?
While their ambulance works in the valley?”
But, a sensible few who, are practical too,
Will not bear with such nonsense much longer
They believe that prevention is better than cure
And their thinking will soon be stronger.
Encourage them, then with your purse, voice and pen
And (while other philanthropists dally)
They will scorn all pretence, and put up a stout fence
On the cliff that hangs over the valley.
The above poem is a forerunner to Camara Jones’ “Cliff” analogy that appears below.
- Camara Jones’ “Cliff analogy”:
Camara Jones’ “cliff analogy” is a useful tool to understand and explain how health inequities arise at different levels in healthcare settings.
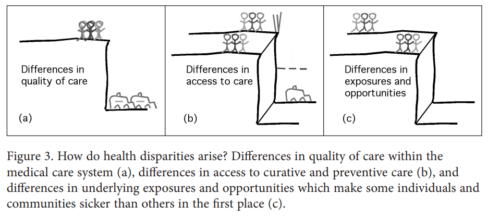
The “cliff” analogy is three-dimensional. The following are the three dimensions;
- Level 1: Differences in exposures and opportunities: The closeness to the cliff of some population groups (“vulnerable groups”) represents the differences in exposures and opportunities for safety.
- Level II: Differences in access to care: The absence of safety nets that prevent falling from the cliff represents the differences in access to care.
- Level III: Differences in Quality of Care: Ambulances below the cliff represent the differences in quality of care after entering a healthcare system such as a hospital.
Then, she gives her approaches:

Image source:
- Change the terminology and narrative
American Medical Association together with the Center for Social Justice published an excellent guide that helps us to change our narrative and language in our journey of popularising health equity concepts. Its preamble begins with this sentence.
” The field of equity, like all other scholarly domains, has developed specific norms that
convey authenticity, precision and meaning”. The guide aims at physicians and healthcare workers”.
Health inequities are produced and sustained by deeply entrenched social systems; we are maintaining them even with our everyday language. That means the unjust systems are embedded without us.
That is why changing our language and narratives matters.
Following are some examples that the document highlights;
| Our daily language | Equity-focused alternative |
| “diabetic” | A person living with diabetes |
| “Homeless” | A person experiencing homelessness |
| “disabled” | A person living with walking difficulty (mention the difficulty here) |
| “COVID-19 cases” | Persons with COVID19 |
| “minorities” | People from (mention the name of the community) |
Further readings
- Government of Canada: Social determinants of health and health inequalities
- About Fair Foundations and promoting equity: VisHealth Framework for Equity: 2015
- CDC health disparities and inequalities report: 2013
- Unequal treatment: Confronting race and ethnic disparities in healthcare, CDC, 2003
- What is health equity?; Robert Wood Jhonson Foundation, 2017
- Health equity series, George Washington University.
- Methods to advance health equity: https://www.youtube.com/watch?v=seHu33_Jf48
- Relfess tool: to analyse your project through the lens of the social inequalities framework
- Social Identities and Systems of Oppression
- Let us talk about moving upstream
- Key health inequalities in Canada, 2018
- 2003 NIH Landmark document on “unequal treatment”
- Ontario 2016 Report on health inequity
- Health Inequities in New Brunswick
- 2013 health disparities report
- Power, politics, and health
- Communities in Action: Pathways to health equity
- Power mapping
- Power mapping organizer training
- Causes of causes: Social determinants of health
- Community health equity builders and a community health equity Charter
- Health equity online course
- Health Equity Toolbox from the University of Delaware
- The Roots of Health Inequity
- Health in All Policies
- Institute for Health Equity
- Social Determinants of Health, WHO
- UN Sustainable Development Group