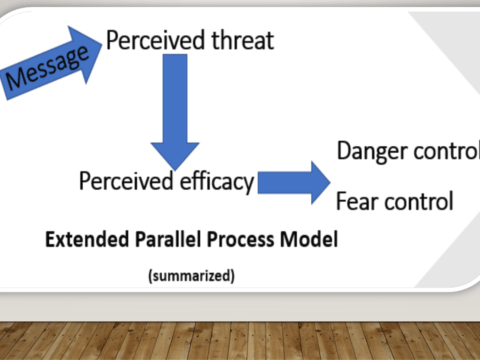
Category: Risk communication
How to frame alcohol policy messages
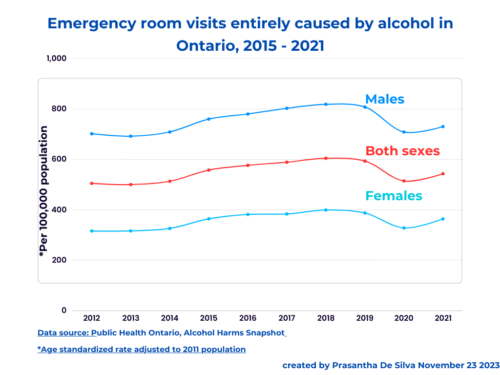
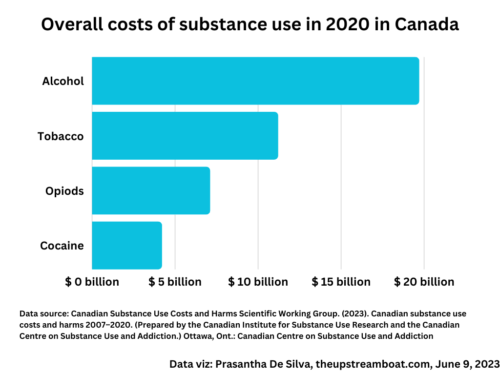
Personal health narrative “Alcohol is bad for your health” We frequently find the above message in the media as a health education message; this is the dominant narrative. In this narrative, we force readers to think about the illnesses that alcohol drinking may cause. This frame results in two unintended consequences: Responsible drinking narrative “Drink responsibly” The industry invariably turns back and says that, This individualistic, neoliberal thinking dominates even in the public health field when it comes to interventions; the most popular intervention is to educate people about the dangers of alcohol consumption and “responsible drinking”; of course, it…
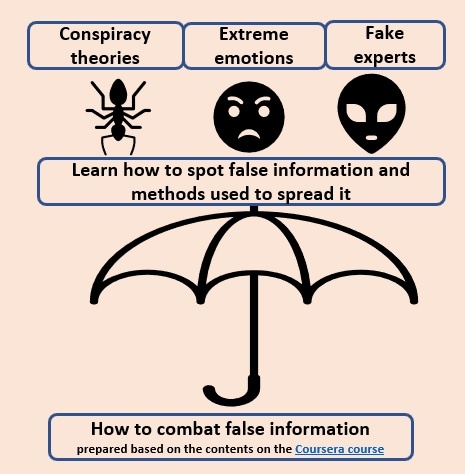
How to deal with COVID19 vaccine hesitancy
COVID 19 vaccine hesitancy is real. It hurts. With Omicron, vaccine hesitancy has become a major roadblock. The problem has gone viral very much like the COVID19 spread. What is COVID 19 vaccine hesitancy? Vaccine hesitancy refers to situations when someone either refuses or delay getting the CVODI19 vaccines. Vaccine hesitancy is not new; it has been there for all vaccines. However, we are discussing this again with this COVID19 pandemic. We have many resources to learn more about it. The latest addition is the Coursera course. It is free. This post dives into this excellent resource. About the course…
COVID-19 can be airborne – Reframe your messages
Evidence is growing that COVID-19 can transmit through air. Need evidence? Julian W Tang et al.’s BMJ article dissects the evidence. Furthermore, governments are changing their health education messages accordingly. In this video clip, the Canadian government are now promoting adequate ventilation as a method of reducing transmission. https://www.youtube.com/watch?v=ZZjTT4nrWu4&t=24s
Is Covid 19 different from the influenza flu?
Even after a year, some are grappling with the same old question: Is Covid 19 different from the seasonal flu? How do we communicate the risk convincingly to this target audience? Obviously, we need to compare number of deaths due to Covid 19 with the number of deaths due to the seasonal flu. The Centre for Risk and Evidence Communication in the University of Cambridge has done exactly that. Look at the following graph; It compares the number of COVID 19 deaths with the deaths from influenza flu and several other common causes. As we can clearly see that the…
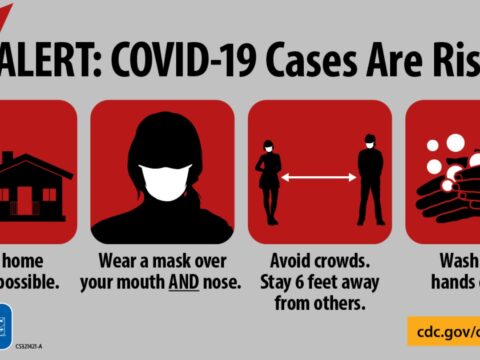
A face mask is not a substitute for physical distancing
A face mask over your mouth AND nose is not a substitute for physical distancing; stay at least 6 feet apart from those who don’t live with you. Messageframing.com #WearAMask over youth mouth AND nose in addition to staying at least 6 feet apart from people who don’t live with you and washing your hands often.
Cover your mouth AND the nose
Cover youth mouth AND nose
Why should we wear a face mask?
Cover your mouth AND nose
When and how to wear a face mask
Even almost a year after the covid19 pandemic, reminding ourselves when and how to wear a face mask continues to become a life-saving activity. Wearing a face mask alone is inadequate to combat this pandemic. However, wearing a face mask is essential to combat this pandemic. This post reminds us of the basic rules of when and how to wear a face mask as recommended by the World Health Organization. How to wear a medical or surgical mask Wash hands before touching the mask cover nose, mouth, and chin (my emphasis: at all times; it cannot be below the nose!…
Avoid traps in risk communication
As an individual who closely follows pandemic communication, I have been observing some communication “traps” that the communicators fall into. During my research on this, I found excellent advice from the US CDC website with regard to this topic. I am sharing relevant pieces from that post here. This post details out dos and don’ts when we communicate events related to an outbreak. Dos Do not s define technical terms in plain language Use language that even a small section cannot understand Ask whether you have made the information clear. Do not assume that everything is clear. use examples or…
Physical distancing is not social distancing
Image source:https://pbs.twimg.com/media/EWCfY8-UwAAdsv_?format=jpg&name=small What we need exactly is to stop spreading the COVID 19 virus; that is it. We do it by staying away from each other physically and adhering to washing hands each time when we touch anything or any surface outside the home and avoid touching face each time after touching anything or any surface outside the home. Certainly, not social distancing; in fact, we should combat social isolation. I am not the only one talking about it. Although a bit late, WHO emphasized its position about it at one of their media conferences, held on March 20, 2020;…